Onze huid, luchtwegen, maagdarmkanaal en urineweg zijn continu in gevecht met micro-organismen, zoals parasieten, bacteriën, schimmels en virussen. De strijd vindt plaats onder regie van ons immuunsysteem dat zich bedient van munitie-onderdelen in de vorm van nutriënten, zoals nitraat (1-3), jodium (4-6), thiocyanaat (5,7,8), selenium (6,9,10) en vitamine C (1-3,11).
Ons maag-darmkanaal staat bekend om zijn microbioom (26). Minder bekend is dat ook de borstklier (12-23), urineweg (24) en prostaat (25) hun eigen microbioom hebben. Bij ontsteking en kanker is de samenstelling van dit microbioom verstoord (12-25).
Microben dringen ons lichaam binnen via de klieren die stoffen afgeven aan onze externe omgeving: de speeksel-, zweet- en traanklieren, maar ook via de gal- en luchtwegen, longen, urineweg, alvleesklier, de vrouwelijke borst en kliertjes in het maag-darmkanaal. In hun holtes en aan- en afvoerwegen vindt het microbioom een prachtig onderkomen.
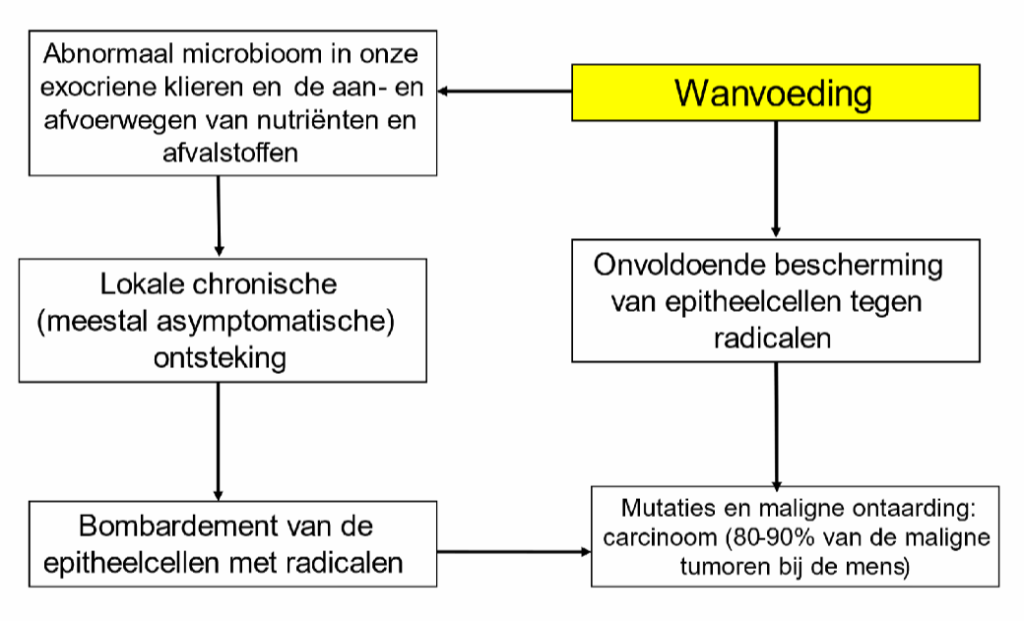
Grotendeels zijn deze microben ‘vriendelijk’ of neutraal. Maar als we ongezond eten neemt hun diversiteit af en stijgt de kans op groei van onvriendelijker soorten: de ziekteverwekkers (27,28). In een lichaam dat acuut of chronisch ontstoken is, veroorzaken microben – maar ook ons immuunsysteem – schade. Onder andere aan ons genetisch materiaal. Er ontstaat een omgeving die gevoelig is voor de ontwikkeling van kwaadaardige cellen (26). Dat de meeste tumoren ontstaan in de binnenbekleding van de bovengenoemde klieren en hun aan- en afvoerwegen naar ‘buiten’ is geen toeval. De zeer actieve ‘epitheelcellen’ in deze bekleding vormen bij kwaadaardige ontaarding een ‘carcinoom’. Deze vorm van kanker maakt 80 tot 90 procent uit van alle kanker bij de mens (28a) en vertoont een sterke relatie met lokale (chronische) infecties.
In cijfers: ontsteking van de prostaat vergroot de kans op prostaatkanker met 14 procent (35,36), een chronische darmontsteking (colitis ulcerosa, ziekte van Crohn; 35,37-39) geeft een 25 procent hogere kans op darmkanker, en ontsteking van de alvleesklier vergroot de kans op alvleesklierkanker wel tien tot twintig keer (35). Borstontsteking verhoogt het risico op borstkanker (40,41). Naar schatting is 20 procent van alle kanker gerelateerd aan chronische infecties, zoals veroorzaakt door de Helicobacter pylori bacterie (maagkanker), het humane papilloma virus (baarmoederhalskanker) en de hepatitis B- en C virussen (leverkanker) (49,51).
In de strijd tussen het immuunsysteem en de microben gaat het er op microniveau hard aan toe. Op de grens met het microbioom maken epitheelcellen reactieve radicalen die zuurstof, stikstof, jodium, zwavel of selenium bevatten (6,7,8,55-58). Hiervoor scheiden de speekselklieren zowel nitraat (61), jodide als hypojodiet (59) uit. De zweetkliertjes doen het met nitraat (64) en gooien daar een schepje vitamine C (62,63) bovenop. Vitamine C helpt in zowel ons maagdarmkanaal als onze urineweg mee met het op afstand houden van microben. Het komt het maagdarmkanaal binnen via de voeding maar ook via kliertjes in de maagwand (69,70, 71,72,73). Voor een vergelijkbaar effect in de urineweg gaat vitamine C er via de urine uit. Dat is dus nuttig en niet ‘zonde van het geld’ (74), zoals populaire criticasters beweren.
Antioxidanten, zoals glutathion, vitamines E en C, en enzymen met koper, zink, mangaan, ijzer of selenium (79) beschermen de epitheelcellen tegen hun eigen geweld.
Om de vrede met het microbioom te bewaren is het van belang om ‘welgevoed’ aan deze chemische strijd te beginnen. Dat doe je met passende hoeveelheden selenium, koper, ijzer, vitamine E en dagelijkse inname van voldoende nitraat, jodium en vitamine C (81-84). Door hun onderlinge reacties buiten de cel voorkomen ze (chronische) infectie, en beperken daarmee eventuele schade en daarmee het lokale ontstaan van kanker. Wie tekorten vermoedt, kan vandaag nog beginnen met betere voeding. Volop verse groenten en fruit (nitraat, vitamine C), en voeding uit de zee voor de broodnodige omega-3 vetzuren, jodium en selenium!
Meer lezen van Frits Muskiet? Bestel dan de columnbundel ‘Wat je niet doodt, maakt je sterker’. Voor leden te koop voor 10,- euro, voor niet-leden te koop voor 17,50.
- Hord NG, Tang Y, Bryan NS. Food sources of nitrates and nitrites: the physiologic context for potential health benefits. Am J Clin Nutr. 2009 Jul;90(1):1-10. doi: 10.3945/ajcn.2008.27131. Epub 2009 May 13. PMID: 19439460.
https://pubmed.ncbi.nlm.nih.gov/19439460
2. Bryan NS, Ahmed S, Lefer DJ, Hord N, von Schwarz ER. Dietary nitrate biochemistry and physiology. An update on clinical benefits and mechanisms of action. Nitric Oxide. 2023 Mar 1;132:1-7. doi: 10.1016/j.niox.2023.01.003. Epub 2023 Jan 20. PMID: 36690137.
https://pubmed.ncbi.nlm.nih.gov/36690137
3. Du J, Filipović MR, Wagner BA, Buettner GR. Ascorbate mediates the non-enzymatic reduction of nitrite to nitric oxide. Adv Redox Res. 2023 Dec;9:100079. doi: 10.1016/j.arres.2023.100079. Epub 2023 Aug 15. PMID: 37692975; PMCID: PMC10486277.
https://pubmed.ncbi.nlm.nih.gov/37692975
4. Fuge, R. (2012). Soils and iodine deficiency. In Essentials of medical geology: revised edition (pp. 417-432). Dordrecht: Springer Netherlands.
https://link.springer.com/chapter/10.1007/978-94-007-4375-5_17
5. De la Vieja A, Santisteban P. Role of iodide metabolism in physiology and cancer. Endocr Relat Cancer. 2018 Apr;25(4):R225-R245. doi: 10.1530/ERC-17-0515. Epub 2018 Feb 1. PMID: 29437784.
https://pubmed.ncbi.nlm.nih.gov/29437784
6. Dijck-Brouwer DAJ, Muskiet FAJ, Verheesen RH, Schaafsma G, Schaafsma A, Geurts JMW. Thyroidal and Extrathyroidal Requirements for Iodine and Selenium: A Combined Evolutionary and (Patho)Physiological Approach. Nutrients. 2022 Sep 20;14(19):3886. doi: 10.3390/nu14193886. PMID: 36235539; PMCID: PMC9571367.
https://pubmed.ncbi.nlm.nih.gov/36235539
7. Patel U, Gingerich A, Widman L, Sarr D, Tripp RA, Rada B. Susceptibility of influenza viruses to hypothiocyanite and hypoiodite produced by lactoperoxidase in a cell-free system. PLoS One. 2018 Jul 25;13(7):e0199167. doi: 10.1371/journal.pone.0199167. PMID: 30044776; PMCID: PMC6059396.
https://pubmed.ncbi.nlm.nih.gov/30044776
8. Bafort F, Parisi O, Perraudin JP, Jijakli MH. Mode of action of lactoperoxidase as related to its antimicrobial activity: a review. Enzyme Res. 2014;2014:517164. doi: 10.1155/2014/517164. Epub 2014 Sep 16. PMID: 25309750; PMCID: PMC4182067.
https://pubmed.ncbi.nlm.nih.gov/25309750
10. Schomburg L. Selenium Deficiency Due to Diet, Pregnancy, Severe Illness, or COVID-19-A Preventable Trigger for Autoimmune Disease. Int J Mol Sci. 2021 Aug 8;22(16):8532. doi: 10.3390/ijms22168532. PMID: 34445238; PMCID: PMC8395178.
https://pubmed.ncbi.nlm.nih.gov/34445238
9. Fordyce, F. M. (2012). Selenium deficiency and toxicity in the environment. In Essentials of medical geology: Revised edition (pp. 375-416). Dordrecht: Springer Netherlands.
https://link.springer.com/chapter/10.1007/978-94-007-4375-5_16
11. Padayatty SJ, Levine M. Vitamin C: the known and the unknown and Goldilocks. Oral Dis. 2016 Sep;22(6):463-93. doi: 10.1111/odi.12446. Epub 2016 Apr 14. PMID: 26808119; PMCID: PMC4959991.
https://pubmed.ncbi.nlm.nih.gov/26808119
12. Urbaniak C, Cummins J, Brackstone M, Macklaim JM, Gloor GB, Baban CK, Scott L, O’Hanlon DM, Burton JP, Francis KP, Tangney M, Reid G. Microbiota of human breast tissue. Appl Environ Microbiol. 2014 May;80(10):3007-14. doi: 10.1128/AEM.00242-14. Epub 2014 Mar 7. PMID: 24610844; PMCID: PMC4018903.
https://pubmed.ncbi.nlm.nih.gov/24610844
13. Latuga MS, Stuebe A, Seed PC. A review of the source and function of microbiota in breast milk. Semin Reprod Med. 2014 Jan;32(1):68-73. doi: 10.1055/s-0033-1361824. Epub 2014 Jan 3. PMID: 24390923.
https://pubmed.ncbi.nlm.nih.gov/24390923
14. Walker WA, Iyengar RS. Breast milk, microbiota, and intestinal immune homeostasis. Pediatr Res. 2015 Jan;77(1-2):220-8. doi: 10.1038/pr.2014.160. Epub 2014 Oct 13. PMID: 25310762.
https://pubmed.ncbi.nlm.nih.gov/25310762
15. Eslami-S Z, Majidzadeh-A K, Halvaei S, Babapirali F, Esmaeili R. Microbiome and Breast Cancer: New Role for an Ancient Population. Front Oncol. 2020 Feb 12;10:120. doi: 10.3389/fonc.2020.00120. PMID: 32117767; PMCID: PMC7028701.
https://pubmed.ncbi.nlm.nih.gov/32117767
16. Kim SY, Yi DY. Components of human breast milk: from macronutrient to microbiome and microRNA. Clin Exp Pediatr. 2020 Aug;63(8):301-309. doi: 10.3345/cep.2020.00059. Epub 2020 Mar 23. PMID: 32252145; PMCID: PMC7402982.
https://pubmed.ncbi.nlm.nih.gov/32252145
17. Laborda-Illanes A, Sanchez-Alcoholado L, Dominguez-Recio ME, Jimenez-Rodriguez B, Lavado R, Comino-Méndez I, Alba E, Queipo-Ortuño MI. Breast and Gut Microbiota Action Mechanisms in Breast Cancer Pathogenesis and Treatment. Cancers (Basel). 2020 Aug 31;12(9):2465. doi: 10.3390/cancers12092465. PMID: 32878124; PMCID: PMC7565530.
https://pubmed.ncbi.nlm.nih.gov/32878124
18. Tzeng A, Sangwan N, Jia M, Liu CC, Keslar KS, Downs-Kelly E, Fairchild RL, Al-Hilli Z, Grobmyer SR, Eng C. Human breast microbiome correlates with prognostic features and immunological signatures in breast cancer. Genome Med. 2021 Apr 16;13(1):60. doi: 10.1186/s13073-021-00874-2. PMID: 33863341; PMCID: PMC8052771.
https://pubmed.ncbi.nlm.nih.gov/33863341
19. Dieleman S, Aarnoutse R, Ziemons J, Kooreman L, Boleij A, Smidt M. Exploring the Potential of Breast Microbiota as Biomarker for Breast Cancer and Therapeutic Response. Am J Pathol. 2021 Jun;191(6):968-982. doi: 10.1016/j.ajpath.2021.02.020. Epub 2021 Mar 10. PMID: 33713687.
https://pubmed.ncbi.nlm.nih.gov/33713687
20. Toumazi D, El Daccache S, Constantinou C. An unexpected link: The role of mammary and gut microbiota on breast cancer development and management (Review). Oncol Rep. 2021 May;45(5):80. doi: 10.3892/or.2021.8031. Epub 2021 Mar 31. PMID: 33786630.
https://pubmed.ncbi.nlm.nih.gov/33786630
21. Feng ZP, Xin HY, Zhang ZW, Liu CG, Yang Z, You H, Xin HW. Gut microbiota homeostasis restoration may become a novel therapy for breast cancer. Invest New Drugs. 2021 Jun;39(3):871-878. doi: 10.1007/s10637-021-01063-z. Epub 2021 Jan 17. PMID: 33454868.
https://pubmed.ncbi.nlm.nih.gov/33454868
22. Wu H, Ganguly S, Tollefsbol TO. Modulating Microbiota as a New Strategy for Breast Cancer Prevention and Treatment. Microorganisms. 2022 Aug 27;10(9):1727. doi: 10.3390/microorganisms10091727. PMID: 36144329; PMCID: PMC9503838.
https://pubmed.ncbi.nlm.nih.gov/36144329
23. Thu MS, Chotirosniramit K, Nopsopon T, Hirankarn N, Pongpirul K. Human gut, breast, and oral microbiome in breast cancer: A systematic review and meta-analysis. Front Oncol. 2023 Mar 17;13:1144021. doi: 10.3389/fonc.2023.1144021. PMID: 37007104; PMCID: PMC10063924.
https://pubmed.ncbi.nlm.nih.gov/37007104
24. Zheng H, Wang C, Yu X, Zheng W, An Y, Zhang J, Zhang Y, Wang G, Qi M, Lin H, Wang F. The Role of Metabolomics and Microbiology in Urinary Tract Infection. Int J Mol Sci. 2024 Mar 8;25(6):3134. doi: 10.3390/ijms25063134. PMID: 38542107; PMCID: PMC10969911.
https://pubmed.ncbi.nlm.nih.gov/38542107
25. Kustrimovic N, Bombelli R, Baci D, Mortara L. Microbiome and Prostate Cancer: A Novel Target for Prevention and Treatment. Int J Mol Sci. 2023 Jan 12;24(2):1511. doi: 10.3390/ijms24021511. PMID: 36675055; PMCID: PMC9860633.
https://pubmed.ncbi.nlm.nih.gov/36675055
26. Anderson SM, Sears CL. The Role of the Gut Microbiome in Cancer: A Review, With Special Focus on Colorectal Neoplasia and Clostridioides difficile. Clin Infect Dis. 2023 Dec 5;77(Suppl 6):S471-S478. doi: 10.1093/cid/ciad640. PMID: 38051969; PMCID: PMC10697667.
https://pubmed.ncbi.nlm.nih.gov/38051969
27. Spragge F, Bakkeren E, Jahn MT, B N Araujo E, Pearson CF, Wang X, Pankhurst L, Cunrath O, Foster KR. Microbiome diversity protects against pathogens by nutrient blocking. Science. 2023 Dec 15;382(6676):eadj3502. doi: 10.1126/science.adj3502. Epub 2023 Dec 15. PMID: 38096285.
https://pubmed.ncbi.nlm.nih.gov/38096285
28. Kumar A, Baruah A, Tomioka M, Iino Y, Kalita MC, Khan M. Caenorhabditis elegans: a model to understand host-microbe interactions. Cell Mol Life Sci. 2020 Apr;77(7):1229-1249. doi: 10.1007/s00018-019-03319-7. Epub 2019 Oct 4. PMID: 31584128.
https://pubmed.ncbi.nlm.nih.gov/31584128
28a. NIH. Cancer Classification
https://training.seer.cancer.gov/disease/categories/classification.html
29. Lowe DB, Storkus WJ. Chronic inflammation and immunologic-based constraints in malignant disease. Immunotherapy. 2011 Oct;3(10):1265-74. doi: 10.2217/imt.11.113. PMID: 21995576; PMCID: PMC3225121.
https://pubmed.ncbi.nlm.nih.gov/21995576
30. Multhoff G, Molls M, Radons J. Chronic inflammation in cancer development. Front Immunol. 2012 Jan 12;2:98. doi: 10.3389/fimmu.2011.00098. PMID: 22566887; PMCID: PMC3342348.
https://pubmed.ncbi.nlm.nih.gov/22566887
31. Greten FR, Grivennikov SI. Inflammation and Cancer: Triggers, Mechanisms, and Consequences. Immunity. 2019 Jul 16;51(1):27-41. doi: 10.1016/j.immuni.2019.06.025. PMID: 31315034; PMCID: PMC6831096.
https://pubmed.ncbi.nlm.nih.gov/31315034
32. Singh N, Baby D, Rajguru JP, Patil PB, Thakkannavar SS, Pujari VB. Inflammation and cancer. Ann Afr Med. 2019 Jul-Sep;18(3):121-126. doi: 10.4103/aam.aam_56_18. PMID: 31417011; PMCID: PMC6704802.
https://pubmed.ncbi.nlm.nih.gov/31417011
33. Zhao H, Wu L, Yan G, Chen Y, Zhou M, Wu Y, Li Y. Inflammation and tumor progression: signaling pathways and targeted intervention. Signal Transduct Target Ther. 2021 Jul 12;6(1):263. doi: 10.1038/s41392-021-00658-5. PMID: 34248142; PMCID: PMC8273155.
https://pubmed.ncbi.nlm.nih.gov/34248142
34. Liu X, Yin L, Shen S, Hou Y. Inflammation and cancer: paradoxical roles in tumorigenesis and implications in immunotherapies. Genes Dis. 2021 Oct 18;10(1):151-164. doi: 10.1016/j.gendis.2021.09.006. PMID: 37013041; PMCID: PMC10066281.
https://pubmed.ncbi.nlm.nih.gov/37013041
35. Rayburn ER, Ezell SJ, Zhang R. Anti-Inflammatory Agents for Cancer Therapy. Mol Cell Pharmacol. 2009;1(1):29-43. doi: 10.4255/mcpharmacol.09.05. PMID: 20333321; PMCID: PMC2843097.
https://pubmed.ncbi.nlm.nih.gov/20333321
36. Jiang J, Li J, Yunxia Z, Zhu H, Liu J, Pumill C. The role of prostatitis in prostate cancer: meta-analysis. PLoS One. 2013 Dec 31;8(12):e85179. doi: 10.1371/journal.pone.0085179. PMID: 24391995; PMCID: PMC3877315.
https://pubmed.ncbi.nlm.nih.gov/24391995
37. Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002 Dec 19-26;420(6917):860-7. doi: 10.1038/nature01322. PMID: 12490959; PMCID: PMC2803035.
https://pubmed.ncbi.nlm.nih.gov/12490959
38. Follin-Arbelet B, Cvancarova Småstuen M, Hovde Ø, Jelsness-Jørgensen LP, Moum B. Risk of Cancer in Patients With Crohn’s Disease 30 Years After Diagnosis (the IBSEN Study). Crohns Colitis 360. 2023 Oct 3;5(4):otad057. doi: 10.1093/crocol/otad057. PMID: 37886706; PMCID: PMC10599393.
https://pubmed.ncbi.nlm.nih.gov/37886706
39. Sun J. Impact of bacterial infection and intestinal microbiome on colorectal cancer development. Chin Med J (Engl). 2022 Jan 27;135(4):400-408. doi: 10.1097/CM9.0000000000001979. PMID: 35089888; PMCID: PMC8869519.
https://pubmed.ncbi.nlm.nih.gov/35089888
40. Chang CM, Lin MC, Yin WY. Risk of breast cancer in women with non-lactational mastitis. Sci Rep. 2019 Oct 30;9(1):15587. doi: 10.1038/s41598-019-52046-3. PMID: 31666573; PMCID: PMC6821708.
https://pubmed.ncbi.nlm.nih.gov/31666573
41. Chen YC, Chan CH, Lim YB, Yang SF, Yeh LT, Wang YH, Chou MC, Yeh CB. Risk of Breast Cancer in Women with Mastitis: A Retrospective Population-Based Cohort Study. Medicina (Kaunas). 2020 Jul 24;56(8):372. doi: 10.3390/medicina56080372. PMID: 32722165; PMCID: PMC7466309.
https://pubmed.ncbi.nlm.nih.gov/32722165
42. Wu C, Zhang Z, Lu Z, Liao M, Zhang Y, Xie Y, Guo X, Yu X, Yang X, Gao Y, Tan A, Mo Z. Prevalence of and risk factors for asymptomatic inflammatory (NIH-IV) prostatitis in Chinese men. PLoS One. 2013 Aug 13;8(8):e71298. doi: 10.1371/journal.pone.0071298. PMID: 23967188; PMCID: PMC3742742.
https://pubmed.ncbi.nlm.nih.gov/23967188
43. Porta C, Larghi P, Rimoldi M, Totaro MG, Allavena P, Mantovani A, Sica A. Cellular and molecular pathways linking inflammation and cancer. Immunobiology. 2009;214(9-10):761-77. doi: 10.1016/j.imbio.2009.06.014. Epub 2009 Jul 17. PMID: 19616341.
https://pubmed.ncbi.nlm.nih.gov/19616341
44. Del Prete A, Allavena P, Santoro G, Fumarulo R, Corsi MM, Mantovani A. Molecular pathways in cancer-related inflammation. Biochem Med (Zagreb). 2011;21(3):264-75. doi: 10.11613/bm.2011.036. PMID: 22420240.
https://pubmed.ncbi.nlm.nih.gov/22420240
45. Zappavigna S, Cossu AM, Grimaldi A, Bocchetti M, Ferraro GA, Nicoletti GF, Filosa R, Caraglia M. Anti-Inflammatory Drugs as Anticancer Agents. Int J Mol Sci. 2020 Apr 9;21(7):2605. doi: 10.3390/ijms21072605. PMID: 32283655; PMCID: PMC7177823.
https://pubmed.ncbi.nlm.nih.gov/32283655
46. Young LS, Rickinson AB. Epstein-Barr virus: 40 years on. Nat Rev Cancer. 2004 Oct;4(10):757-68. doi: 10.1038/nrc1452. PMID: 15510157.
https://pubmed.ncbi.nlm.nih.gov/15510157
47. Disanto G, Pakpoor J, Morahan JM, Hall C, Meier UC, Giovannoni G, Ramagopalan SV. Epstein-Barr virus, latitude and multiple sclerosis. Mult Scler. 2013 Mar;19(3):362-5. doi: 10.1177/1352458512451942. Epub 2012 Jul 5. PMID: 22767435.
https://pubmed.ncbi.nlm.nih.gov/22767435
48. Esau D. Viral Causes of Lymphoma: The History of Epstein-Barr Virus and Human T-Lymphotropic Virus 1. Virology (Auckl). 2017 Sep 25;8:1178122X17731772. doi: 10.1177/1178122X17731772. PMID: 28983187; PMCID: PMC5621661.
https://pubmed.ncbi.nlm.nih.gov/28983187
49. Mui UN, Haley CT, Vangipuram R, Tyring SK. Human oncoviruses: Mucocutaneous manifestations, pathogenesis, therapeutics, and prevention: Hepatitis viruses, human T-cell leukemia viruses, herpesviruses, and Epstein-Barr virus. J Am Acad Dermatol. 2019 Jul;81(1):23-41. doi: 10.1016/j.jaad.2018.10.072. Epub 2018 Nov 29. PMID: 30502415.
https://pubmed.ncbi.nlm.nih.gov/30502415
50. Ruiz-Pablos M, Paiva B, Montero-Mateo R, Garcia N, Zabaleta A. Epstein-Barr Virus and the Origin of Myalgic Encephalomyelitis or Chronic Fatigue Syndrome. Front Immunol. 2021 Nov 15;12:656797. doi: 10.3389/fimmu.2021.656797. PMID: 34867935; PMCID: PMC8634673.
https://pubmed.ncbi.nlm.nih.gov/34867935
51. Hibino S, Kawazoe T, Kasahara H, Itoh S, Ishimoto T, Sakata-Yanagimoto M, Taniguchi K. Inflammation-Induced Tumorigenesis and Metastasis. Int J Mol Sci. 2021 May 21;22(11):5421. doi: 10.3390/ijms22115421. PMID: 34063828; PMCID: PMC8196678.
https://pubmed.ncbi.nlm.nih.gov/34063828
52. Rogers J. The inflammatory response in Alzheimer’s disease. J Periodontol. 2008 Aug;79(8 Suppl):1535-43. doi: 10.1902/jop.2008.080171. PMID: 18673008.
https://pubmed.ncbi.nlm.nih.gov/18673008
53. Lewis, M. D. (2017). Use of Omega-3s in Traumatic Brain Injury. Clin Surg. 2017; 2, 1449.
https://www.clinicsinsurgery.com/open-access/use-of-omega-3s-in-traumatic-brain-injury-2889.pdf
54. Laforge M, Elbim C, Frère C, Hémadi M, Massaad C, Nuss P, Benoliel JJ, Becker C. Tissue damage from neutrophil-induced oxidative stress in COVID-19. Nat Rev Immunol. 2020 Sep;20(9):515-516. doi: 10.1038/s41577-020-0407-1. Erratum in: Nat Rev Immunol. 2020 Aug 10;: PMID: 32728221; PMCID: PMC7388427.
https://pubmed.ncbi.nlm.nih.gov/32728221
55. Mazumdar A, Adak S, Chatterjee R, Banerjee RK. Mechanism-based inactivation of lacrimal-gland peroxidase by phenylhydrazine: a suicidal substrate to probe the active site. Biochem J. 1997 Jun 15;324 ( Pt 3)(Pt 3):713-9. doi: 10.1042/bj3240713. PMID: 9210393; PMCID: PMC1218485.
https://pubmed.ncbi.nlm.nih.gov/9210393
56. Derscheid RJ, van Geelen A, Berkebile AR, Gallup JM, Hostetter SJ, Banfi B, McCray PB Jr, Ackermann MR. Increased concentration of iodide in airway secretions is associated with reduced respiratory syncytial virus disease severity. Am J Respir Cell Mol Biol. 2014 Feb;50(2):389-97. doi: 10.1165/rcmb.2012-0529OC. PMID: 24053146; PMCID: PMC3930944.
https://pubmed.ncbi.nlm.nih.gov/24053146
57. Aydogan F, Ayhan Tuzcu E, Aydogan A, Akkucuk S, Coskun M, Ustun I, Gökçe C. Effect of radioactive iodine therapy on lacrimal gland functions in patients with hyperthyroidism. Clin Nucl Med. 2014 Apr;39(4):315-8. doi: 10.1097/RLU.0000000000000308. PMID: 24300361.
https://pubmed.ncbi.nlm.nih.gov/24300361
58. Smith ML, Sharma S, Singh TP. Iodide supplementation of the anti-viral duox-lactoperoxidase activity may prevent some SARS-CoV-2 infections. Eur J Clin Nutr. 2022 Apr;76(4):629-630. doi: 10.1038/s41430-021-00995-2. Epub 2021 Sep 1. PMID: 34471253; PMCID: PMC8408568.
https://pubmed.ncbi.nlm.nih.gov/34471253
59. Akiba Y, Leung AM, Bashir MT, Ebrahimi R, Currier JW, Neverova N, Kaunitz JD. Excess iodine exposure acutely increases salivary iodide and antimicrobial hypoiodous acid concentrations in humans. Sci Rep. 2022 Dec 3;12(1):20935. doi: 10.1038/s41598-022-23803-8. PMID: 36463312; PMCID: PMC9719529.
https://pubmed.ncbi.nlm.nih.gov/36463312
60. Salmin VV, Morgun AV, Olovyannikova RY, Kutyakov VA, Lychkovskaya EV, Brusina EB, Salmina AB. Atmospheric Reactive Oxygen Species and Some Aspects of the Antiviral Protection at the Respiratory Epithelium. Biochem Mosc Suppl B Biomed Chem. 2022;16(2):79-90. doi: 10.1134/S1990750822020068. Epub 2022 May 17. PMID: 35601461; PMCID: PMC9113385.
https://pubmed.ncbi.nlm.nih.gov/35601461
61. Zhang H, Qin L. Positive feedback loop between dietary nitrate intake and oral health. Nutr Res. 2023 Jul;115:1-12. doi: 10.1016/j.nutres.2023.04.008. Epub 2023 Apr 29. PMID: 37207592
https://pubmed.ncbi.nlm.nih.gov/37207592
62. Tang YM, Wang DG, Li J, Li XH, Wang Q, Liu N, Liu WT, Li YX. Relationships between micronutrient losses in sweat and blood pressure among heat-exposed steelworkers. Ind Health. 2016 Jun 10;54(3):215-23. doi: 10.2486/indhealth.2014-0225. Epub 2016 Apr 16. PMID: 27087421; PMCID: PMC4939859.
https://pubmed.ncbi.nlm.nih.gov/27087421
63. Wang L, Pan L, Han X, Ha MN, Li K, Yu H, Zhang Q, Li Y, Hou C, Wang H. A portable ascorbic acid in sweat analysis system based on highly crystalline conductive nickel-based metal-organic framework (Ni-MOF). J Colloid Interface Sci. 2022 Jun 15;616:326-337. doi: 10.1016/j.jcis.2022.02.058. Epub 2022 Feb 16. PMID: 35219198.
https://pubmed.ncbi.nlm.nih.gov/35219198
64. Weller R, Pattullo S, Smith L, Golden M, Ormerod A, Benjamin N. Nitric oxide is generated on the skin surface by reduction of sweat nitrate. J Invest Dermatol. 1996 Sep;107(3):327-31. doi: 10.1111/1523-1747.ep12363167. PMID: 8751965.
https://pubmed.ncbi.nlm.nih.gov/8751965
65. Herb M, Schramm M. Functions of ROS in Macrophages and Antimicrobial Immunity. Antioxidants (Basel). 2021 Feb 19;10(2):313. doi: 10.3390/antiox10020313. PMID: 33669824; PMCID: PMC7923022.
https://pubmed.ncbi.nlm.nih.gov/33669824
66. Thomas DC. The phagocyte respiratory burst: Historical perspectives and recent advances. Immunol Lett. 2017 Dec;192:88-96. doi: 10.1016/j.imlet.2017.08.016. Epub 2017 Aug 31. PMID: 28864335.
https://pubmed.ncbi.nlm.nih.gov/28864335
67. Respiratory burst. Wikipedia, accessed 09 April 2024
https://en.wikipedia.org/wiki/Respiratory_burst
68. Muskiet FAJ. Je hebt ze niet nodig en ze kunnen nog schadelijk zijn ook. Supplementen deel 1. Voedingsgeneeskunde 2024;25(1)34-41
https://www.voedingsgeneeskunde.nl/vg-25-1/hebt-nodig-kunnen-nog-schadelijk-zijn-ook
69. Kaźmierczak-Barańska J, Boguszewska K, Adamus-Grabicka A, Karwowski BT. Two Faces of Vitamin C-Antioxidative and Pro-Oxidative Agent. Nutrients. 2020 May 21;12(5):1501. doi: 10.3390/nu12051501. PMID: 32455696; PMCID: PMC7285147.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7285147
70. Levine M, Padayatty SJ, Espey MG. Vitamin C: a concentration-function approach yields pharmacology and therapeutic discoveries. Adv Nutr. 2011 Mar;2(2):78-88. doi: 10.3945/an.110.000109. Epub 2011 Mar 10. PMID: 22332036; PMCID: PMC3065766.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3065766/50. Padayatty SJ, Levine M. Vitamin C: the known and the unknown and Goldilocks. Oral Dis. 2016 Sep;22(6):463-93. doi: 10.1111/odi.12446. Epub 2016 Apr 14. PMID: 26808119; PMCID: PMC4959991.
https://pubmed.ncbi.nlm.nih.gov/26808119
71. Yamasaki H, Imai H, Tanaka A, Otaki JM. Pleiotropic Functions of Nitric Oxide Produced by Ascorbate for the Prevention and Mitigation of COVID-19: A Revaluation of Pauling’s Vitamin C Therapy. Microorganisms. 2023 Feb 3;11(2):397. doi: 10.3390/microorganisms11020397. PMID: 36838362; PMCID: PMC9963342.
https://pubmed.ncbi.nlm.nih.gov/36838362
72. Zhang H, Qin L. Positive feedback loop between dietary nitrate intake and oral health. Nutr Res. 2023 Jul;115:1-12. doi: 10.1016/j.nutres.2023.04.008. Epub 2023 Apr 29. PMID: 37207592
https://pubmed.ncbi.nlm.nih.gov/37207592
73. Hickling DR, Nitti VW. Management of recurrent urinary tract infections in healthy adult women. Rev Urol. 2013;15(2):41-8. PMID: 24082842; PMCID: PMC3784967.
https://pubmed.ncbi.nlm.nih.gov/24082842
74. RADAR in coproductie met het Voedingscentrum. Vitaminepillen, potje onzin of toch niet?, Accessed 30-12-2023
Vitaminepillen, potje onzin of toch niet? – RADAR+ (radarplus.nl)
75. Institute of Medicine (US) Panel on Dietary Antioxidants and Related Compounds. Dietary Reference Intakes for Vitamin C, Vitamin E, Selenium, and Carotenoids. Washington (DC): National Academies Press (US); 2000.
https://www.ncbi.nlm.nih.gov/books/NBK225483/pdf/Bookshelf_NBK225483.pdf
76. Carr AC, Lykkesfeldt J. Discrepancies in global vitamin C recommendations: a review of RDA criteria and underlying health perspectives. Crit Rev Food Sci Nutr. 2021;61(5):742-755. doi: 10.1080/10408398.2020.1744513. Epub 2020 Mar 30. PMID: 32223303.
https://pubmed.ncbi.nlm.nih.gov/32223303
77. King, G., Beins, M., Larkin, J., Summers, B., & Ordman, A. B. (1994). Rate of excretion of vitamin C in human urine. Age, 17, 87-92.
https://link.springer.com/article/10.1007/BF02435011
78. Lindblad M, Tveden-Nyborg P, Lykkesfeldt J. Regulation of vitamin C homeostasis during deficiency. Nutrients. 2013 Jul 25;5(8):2860-79. doi: 10.3390/nu5082860. PMID: 23892714; PMCID: PMC3775232.
https://pubmed.ncbi.nlm.nih.gov/23892714
78a. Lee, W. J. (2019). Vitamin c in human health and disease: Effects, mechanisms of action, and new guidance on intake. Springer.
https://link.springer.com/book/10.1007/978-94-024-1713-5
78b. Milton K. Micronutrient intakes of wild primates: are humans different? Comp Biochem Physiol A Mol Integr Physiol. 2003 Sep;136(1):47-59. doi: 10.1016/s1095-6433(03)00084-9. PMID: 14527629.
https://pubmed.ncbi.nlm.nih.gov/14527629
79. Matés JM, Pérez-Gómez C, Núñez de Castro I. Antioxidant enzymes and human diseases. Clin Biochem. 1999 Nov;32(8):595-603. doi: 10.1016/s0009-9120(99)00075-2. PMID: 10638941.
https://pubmed.ncbi.nlm.nih.gov/10638941
80. Stoutjesdijk E, Schaafsma A, Dijck-Brouwer DAJ, Muskiet FAJ. Iodine status during pregnancy and lactation: a pilot study in the Netherlands. Neth J Med. 2018 Jul;76(5):210-217. PMID: 30019676.
https://pubmed.ncbi.nlm.nih.gov/30019676
81. Mayunga KC, Lim-A-Po M, Lubberts J, Stoutjesdijk E, Touw DJ, Muskiet FAJ, Dijck-Brouwer DAJ. Pregnant Dutch Women Have Inadequate Iodine Status and Selenium Intake. Nutrients. 2022 Sep 22;14(19):3936. doi: 10.3390/nu14193936. PMID: 36235589; PMCID: PMC9572179.
https://pubmed.ncbi.nlm.nih.gov/36235589
82. Muskiet FAJ, Schaafsma G, Dijck-Brouwer DAJ. Nederland is nu ook officieel seleniumdeficiënt. Voedingsgeneeskunde 2023;24(6)70-71
https://www.voedingsgeneeskunde.nl/vg-24-6/nederland-nu-ook-officieel-seleniumdefici%C3%ABnt
83. Verkaik-Kloosterman, J., van Rossum, C., Beukers, M., & Buurma-Rethans, E. (2018). The habitual micronutrient intake of Dutch adults (VCP 2007-2010) compared with dietary reference values set by the Health Council of the Netherlands (2014) and EFSA (2010-2017).
https://www.rivm.nl/sites/default/files/2018-11/Memo_habitualmicronutintakeVCP0710_vs1.pdf
84. Kaczor, T. (2014). Iodine and cancer a summary of the evidence to date. Nat Med J, 6(6), 2014-06.
https://www.naturalmedicinejournal.com/journal/iodine-and-cancer
85. Schrauzer GN, White DA, Schneider CJ. Cancer mortality correlation studies–III: statistical associations with dietary selenium intakes. Bioinorg Chem. 1977;7(1):23-31. doi: 10.1016/s0006-3061(00)80126-x. PMID: 856291.
https://pubmed.ncbi.nlm.nih.gov/856291
86. Shimizu H, Ross RK, Bernstein L, Yatani R, Henderson BE, Mack TM. Cancers of the prostate and breast among Japanese and white immigrants in Los Angeles County. Br J Cancer. 1991 Jun;63(6):963-6. doi: 10.1038/bjc.1991.210. PMID: 2069852; PMCID: PMC1972548.
https://pubmed.ncbi.nlm.nih.gov/2069852
87. Koletzko B, Boey CC, Campoy C, Carlson SE, Chang N, Guillermo-Tuazon MA, Joshi S, Prell C, Quak SH, Sjarif DR, Su Y, Supapannachart S, Yamashiro Y, Osendarp SJ. Current information and Asian perspectives on long-chain polyunsaturated fatty acids in pregnancy, lactation, and infancy: systematic review and practice recommendations from an early nutrition academy workshop. Ann Nutr Metab. 2014;65(1):49-80. doi: 10.1159/000365767. Epub 2014 Sep 16. PMID: 25227906.
https://pubmed.ncbi.nlm.nih.gov/25227906
88. Hallberg, Ö., Huttunen, P., & Johansson, O. (2014). Cancer incidence vs. population average sleep duration on spring mattresses. Adv. Stud. Med. Sci, 2, 17-30.
https://electromagnetichealth.org/wp-content/uploads/2015/01/Hallberg_et_al._2014b.pdf
89. Kimura T, Egawa S. Epidemiology of prostate cancer in Asian countries. Int J Urol. 2018 Jun;25(6):524-531. doi: 10.1111/iju.13593. Epub 2018 May 8. PMID: 29740894.
https://pubmed.ncbi.nlm.nih.gov/29740894
90. Miller, D. W. (2006). Extrathyroidal benefits of iodine. Journal of American Physicians and Surgeons, 11(4), 106.
91. Oster O, Schmiedel G, Prellwitz W. The organ distribution of selenium in German adults. Biol Trace Elem Res. 1988 Jan-Apr;15:23-45. doi: 10.1007/BF02990125. PMID: 2484520.
https://pubmed.ncbi.nlm.nih.gov/2484520
92. Zhou BF, Stamler J, Dennis B, Moag-Stahlberg A, Okuda N, Robertson C, Zhao L, Chan Q, Elliott P; INTERMAP Research Group. Nutrient intakes of middle-aged men and women in China, Japan, United Kingdom, and United States in the late 1990s: the INTERMAP study. J Hum Hypertens. 2003 Sep;17(9):623-30. doi: 10.1038/sj.jhh.1001605. PMID: 13679952; PMCID: PMC6561109.
https://pubmed.ncbi.nlm.nih.gov/13679952
93. Zava TT, Zava DT. Assessment of Japanese iodine intake based on seaweed consumption in Japan: A literature-based analysis. Thyroid Res. 2011 Oct 5;4:14. doi: 10.1186/1756-6614-4-14. PMID: 21975053; PMCID: PMC3204293.
https://pubmed.ncbi.nlm.nih.gov/21975053
94. Fuse Y, Ito Y, Shishiba Y, Irie M. Current Iodine Status in Japan: A Cross-sectional Nationwide Survey of Schoolchildren, 2014-2019. J Clin Endocrinol Metab. 2022 Apr 19;107(5):e2065-e2079. doi: 10.1210/clinem/dgab919. PMID: 34935958.
https://pubmed.ncbi.nlm.nih.gov/34935958
95. Institute of Medicine (US) Panel on Micronutrients. Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc; The National Academic Press: Washington, DC, USA, 2001.
https://pubmed.ncbi.nlm.nih.gov/25057538
96. Overview on Tolerable Upper Intake Levels as derived by the Scientific Committee on Food (SCF) and the EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA)
https://www.efsa.europa.eu/sites/default/files/assets/UL_Summary_tables.pdf
97. Noahsen P, Kleist I, Larsen HM, Andersen S. Intake of seaweed as part of a single sushi meal, iodine excretion and thyroid function in euthyroid subjects: a randomized dinner study. J Endocrinol Invest. 2020 Apr;43(4):431-438. doi: 10.1007/s40618-019-01122-6. Epub 2019 Sep 30. PMID: 31571150.
https://pubmed.ncbi.nlm.nih.gov/31571150
98. Jin YJ, Kwon MJ, Kim JH, Kim JH, Choi HG. Association between Thyroid Cancer and Breast Cancer: Two Longitudinal Follow-Up Studies Using a National Health Screening Cohort. J Pers Med. 2022 Jan 20;12(2):133. doi: 10.3390/jpm12020133. PMID: 35207622; PMCID: PMC8880453.
https://pubmed.ncbi.nlm.nih.gov/35207622
99. Manjer J, Sandsveden M, Borgquist S. Serum Iodine and Breast Cancer Risk: A Prospective Nested Case-Control Study Stratified for Selenium Levels. Cancer Epidemiol Biomarkers Prev. 2020 Jul;29(7):1335-1340. doi: 10.1158/1055-9965.EPI-20-0122. Epub 2020 May 26. PMID: 32457181.
https://pubmed.ncbi.nlm.nih.gov/32457181
100. Szwiec M, Marciniak W, Derkacz R, Huzarski T, Gronwald J, Cybulski C, Dębniak T, Jakubowska A, Lener M, Falco M, Kładny J, Baszuk P, Duszyński J, Kotsopoulos J, Narod SA, Lubiński J. Serum Selenium Level Predicts 10-Year Survival after Breast Cancer. Nutrients. 2021 Mar 16;13(3):953. doi: 10.3390/nu13030953. PMID: 33809461; PMCID: PMC7998294.
https://pubmed.ncbi.nlm.nih.gov/33809461
101. Moreno-Vega A, Vega-Riveroll L, Ayala T, Peralta G, Torres-Martel JM, Rojas J, Mondragón P, Domínguez A, De Obaldía R, Avecilla-Guerrero C, Anguiano B, Delgado-González E, Zambrano-Estrada X, Cuenca-Micó O, De La Puente Flores O, Varela-Echavarría A, Aceves C. Adjuvant Effect of Molecular Iodine in Conventional Chemotherapy for Breast Cancer. Randomized Pilot Study. Nutrients. 2019 Jul 17;11(7):1623. doi: 10.3390/nu11071623. PMID: 31319484; PMCID: PMC6682905.
https://pubmed.ncbi.nlm.nih.gov/31319484
102. Anguiano B, Álvarez L, Delgado-González E, Ortiz-Martínez Z, Montes de Oca C, Morales G, Aceves C. Protective effects of iodine on rat prostate inflammation induced by sex hormones and on the DU145 prostate cancer cell line treated with TNF. Mol Cell Endocrinol. 2023 Jul 15;572:111957. doi: 10.1016/j.mce.2023.111957. Epub 2023 May 14. PMID: 37192707.
https://pubmed.ncbi.nlm.nih.gov/37192707
103. Aceves C, Anguiano B, Delgado G. The extrathyronine actions of iodine as antioxidant, apoptotic, and differentiation factor in various tissues. Thyroid. 2013 Aug;23(8):938-46. doi: 10.1089/thy.2012.0579. PMID: 23607319; PMCID: PMC3752513.
https://pubmed.ncbi.nlm.nih.gov/23607319
104. Cavalieri RR. Iodine metabolism and thyroid physiology: current concepts. Thyroid. 1997 Apr;7(2):177-81. doi: 10.1089/thy.1997.7.177. PMID: 9133680.
https://pubmed.ncbi.nlm.nih.gov/9133680
105. Bai XY, Qu X, Jiang X, Xu Z, Yang Y, Su Q, Wang M, Wu H. Association between Dietary Vitamin C Intake and Risk of Prostate Cancer: A Meta-analysis Involving 103,658 Subjects. J Cancer. 2015 Jul 28;6(9):913-21. doi: 10.7150/jca.12162. PMID: 26284143; PMCID: PMC4532989.
https://pubmed.ncbi.nlm.nih.gov/26284143
106. Bourdoux P, Delange F, Gerard M, Mafuta M, Hanson A, Ermans AM. Evidence that cassava ingestion increases thiocyanate formation: a possible etiologic factor in endemic goiter. J Clin Endocrinol Metab. 1978 Apr;46(4):613-21. doi: 10.1210/jcem-46-4-613. PMID: 755045.
https://pubmed.ncbi.nlm.nih.gov/755045
107. Ravera S, Reyna-Neyra A, Ferrandino G, Amzel LM, Carrasco N. The Sodium/Iodide Symporter (NIS): Molecular Physiology and Preclinical and Clinical Applications. Annu Rev Physiol. 2017 Feb 10;79:261-289. doi: 10.1146/annurev-physiol-022516-034125. PMID: 28192058; PMCID: PMC5739519.
https://pubmed.ncbi.nlm.nih.gov/28192058
108. Calder PC, Carr AC, Gombart AF, Eggersdorfer M. Optimal Nutritional Status for a Well-Functioning Immune System Is an Important Factor to Protect against Viral Infections. Nutrients. 2020 Apr 23;12(4):1181. doi: 10.3390/nu12041181. PMID: 32340216; PMCID: PMC7230749.
https://pubmed.ncbi.nlm.nih.gov/32340216
109. Gombart AF, Pierre A, Maggini S. A Review of Micronutrients and the Immune System-Working in Harmony to Reduce the Risk of Infection. Nutrients. 2020 Jan 16;12(1):236. doi: 10.3390/nu12010236. PMID: 31963293; PMCID: PMC7019735.
https://pubmed.ncbi.nlm.nih.gov/31963293
110. Schomburg L. Selenium Deficiency Due to Diet, Pregnancy, Severe Illness, or COVID-19-A Preventable Trigger for Autoimmune Disease. Int J Mol Sci. 2021 Aug 8;22(16):8532. doi: 10.3390/ijms22168532. PMID: 34445238; PMCID: PMC8395178.
https://pubmed.ncbi.nlm.nih.gov/34445238
111. Blomhoff, R., Andersen, R., Arnesen, E. K., Christensen, J. J., Eneroth, H., Erkkola, M., … & Trolle, E. (2023). Nordic Nutrition Recommendations 2023: Integrating Environmental Aspects.
https://www.diva-portal.org/smash/record.jsf?dswid=-4899&pid=diva2%3A1769986
MMV maakt wekelijks een selectie uit het nieuws over voeding en leefstijl in relatie tot kanker en andere medische condities.
Inschrijven nieuwsbrief